Hot Tech for Cold Cancers: How Microwave Imaging Is Reinventing Breast Screening
Disclaimer: this is an AI-generated article intended to highlight interesting concepts / methods / tools used within the SmartDATA Lab's research. This is for educating lab members as well as general readers interested in the lab. The article may contain errors.
Why sending low-energy waves into your chest might be the next mammogram—and the math behind making it work
Picture your chest as a crowded subway car: packed, complicated, and full of different signals—some harmless, others alarming. Traditional mammography snapshots it like a grainy train schedule. Enter microwave imaging, which floods this crowded space with gentle electromagnetic pulses (1–10 GHz), listens to how they bounce back, and pieces together a map of tissue properties. It’s like a radar that detects suspicious riders without shaming them for squeezing on too tight.
Microwave imaging for breast cancer combines electromagnetics, inverse problems, and signal processing—a playground for math nerds who want to turn reflections into medical breakthroughs. And behind much of this progress are longtime efforts at McGill University and newer advances from the University of Utah. Let’s unpack how it all works—and why it’s still struggling to go mainstream today.
The Electromagnetic Stack: How We Hear Tumors in Microwaves
When microwaves enter the body, they slow down in fatty, watery, or dense tissues. These dielectric contrasts create reflections that can be mathematically modeled by Maxwell’s equations. In practice, most imaging systems use a simplified discrete forward model: Erecv=A(εr,σ) EtransE_{\text{recv}} = A(\varepsilon_r,\sigma)\,E_{\text{trans}}Erecv=A(εr,σ)Etrans
Here, AAA is a large matrix relating tissue permittivity εr\varepsilon_rεr and conductivity σ\sigmaσ to received signals. Solving the inverse problem—estimating εr(x)\varepsilon_r(x)εr(x) from noisy, limited measurements—is a classic ill-conditioned system in numerical linear algebra.
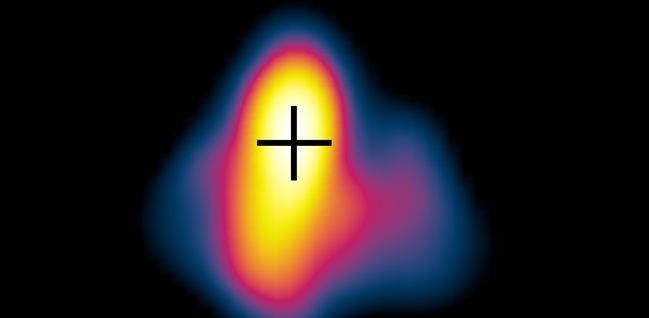
Popular reconstruction methods include Gauss–Newton iterations and regularized linear solvers (like Tikhonov). For radar-based approaches, delay-and-sum beamforming aligns time-shifted signals to focus energy on suspected spots. But both suffer when there’s noise, limited antenna coverage, or tissue complexity.
Math in Action: Sorting Waves from Noise
To make microwave imaging useful in clinics, we must wrestle with math—and uncertainty:
- Sparse linear algebra: Many wave interactions are weak; only a few are relevant. By solving under-determined systems with L1 regularization, algorithms sparsify the solution and isolate tumor signals.
- Multifrequency inversion: Stacking data across frequency bands forms tall, skinny matrix systems; regularization relies on singular values to avoid amplifying noise.
- Beamforming power: In radar confocal imaging, time-shifted signals are summed to pinpoint reflections. Mathematically, this is a matrix–vector multiply using shifted identity blocks—a computationally cheap method for real-time imaging.
These techniques also borrow from signal processing in radar and immune ultrasound—minimum variance adaptive beamformers, MUSIC algorithms, and eigenvalue analyses all show up.
From Echoes to Evidence: Calibration Matters
A prototype from McGill demonstrated that microwave radar could detect malignant lumps in controlled settings by solving a time-domain reflectometry equation and calibrating against known targets. But translating that to noisy, heterogeneous breasts is hard.
The University of Utah’s recent work addresses this by modeling dielectric variability—how breast tissue properties change with age, hydration, or genetics. Sensitivity matrices show how small permittivity errors shift tumor location estimates, pushing researchers to embed variability modeling and uncertainty quantification in the inversion process.
Why It Still Isn’t Everywhere
Despite early promises, microwave imaging isn’t yet a household name. Here’s why:
- Solving ill-posed systems: Reconstructing dielectric maps from limited data is hard. Regularizing the wrong way yields blurry images and missed tumors.
- Image-quality standards: Many studies focus on tumor detection rates, but neglect metrics like resolution, contrast, and false-positives—essential in clinical diagnostics.
- Equipment variability: Different antenna arrays yield different sensitivities. Unless calibrated per session, results fluctuate.
- Machine learning hype: ML can classify tumor vs. non‑tumor signatures but often requires large, labeled datasets. Guarding against overfitting with small samples is tricky.
The Road Ahead: Smarter Math, Smarter Imaging
Here’s how the field hopes to win:
- Physics-informed AI: Hybrid models combine Maxwell’s forward model with learned inversion maps, ensuring predictions respect physics while adapting to real data.
- Uncertainty quantification: Embedding error bounds (via Bayesian solvers) gives confidence to diagnoses—crucial in medical settings.
- Pilot clinical studies: The University of Utah team is running trials with patient-specific calibration to test feasibility in “real-world breast varieties.”
The Bottom Line
Microwave breast imaging is a bold challenger to X‑rays and MRI: non-ionizing, portable, and potentially cheap. But getting from radar reflections to clinical decisions demands strong linear algebra, physics-informed math, and clinical rigor. The next 5 years will test whether clever math can finally tip the scale—and help detect cancers without compressing chests or scaring patients.
Key References on Microwave Breast Cancer Imaging
- Kwon S., Lee S. (2016). Instantaneous microwave imaging with time-domain measurements for breast cancer detection. Electronics Letters, 49(10), 653–654.
https://doi.org/10.1049/el.2013.0248 - Hall K., Furse C. (2025). Evaluating the impact of tissue dielectric property variability on microwave imaging for breast cancer detection. IEEE APS/URSI conference.
Conference presentation listing - Modiri A., Goudreau S., Rahimi A., Kiasaleh K. (2017). Review of breast screening: Toward clinical realization of microwave imaging. Medical Physics, 44(12), e446–e458.
https://doi.org/10.1002/mp.12611 - Reimer T., Pistorius S. (2023). Review of tumour detection and image quality analysis in experimental breast microwave sensing. Sensors, 23(11), 5123.
https://doi.org/10.3390/s23115123 - Porter, E., Santorelli, A., Coates, M., Popović, M. (2013). Time-domain microwave breast cancer detection: extensive system testing with phantoms. Technol Cancer Res Treat., 12(2), 131–143.
https://doi.org/10.7785/tcrt.2012.500307
electromagnetics Imaging Inverse Problem Physical Mismatch Signal Processing